Cervical Foraminal Disc Herniation Adjacent to a Fused Segment
Dr. Jeff Golan
Dr. Oded Rabau
McGill University, Montréal, Quebec, Canada
History
79 y/o healthy male presented with a 4-week history of spontaneous incapacitating shoulder pain radiating down the right arm to the hand in a typical C8 dermatomal distribution. He also reported numbness and weakness in the hand with no improvement since symptom onset. He had remote C6-7 anterior discectomy and uninstrumented fusion.
Examination
The patient is unable to fully extend his fingers and the hand is in a claw-like posture. There is no apparent interossei function. His sensory function along the C8 and some of the C7 dermatomes is quite reduced.
Imaging
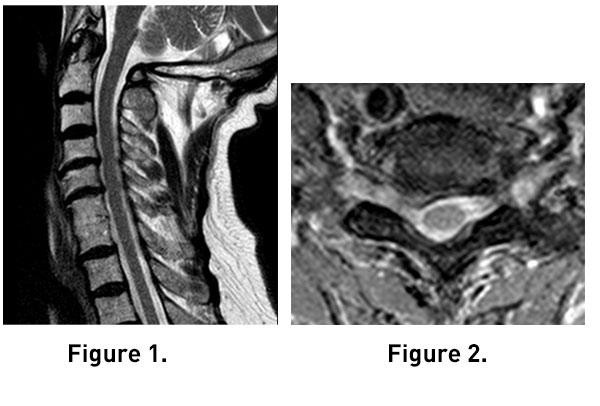
MRI T2W sagittal (Fig. 1) and axial images (Fig. 2,3) reveal right C7-T1 foraminal disc herniation or extrusion. The C6-7disc space is solidly fused. The quality of images is degraded by movement artifact given the patient’s pain.
Diagnosis
79 y/o male with subacute C8 radiculopathy due to C7-T1 foraminal disc herniation adjacent to a C6-7 fused segment.
Treatment
Goal: Decompress the C8 root
Challenge: Anterior approach through prior surgical corridor/scar tissue and extending fusion versus posterior approach with or without fusion
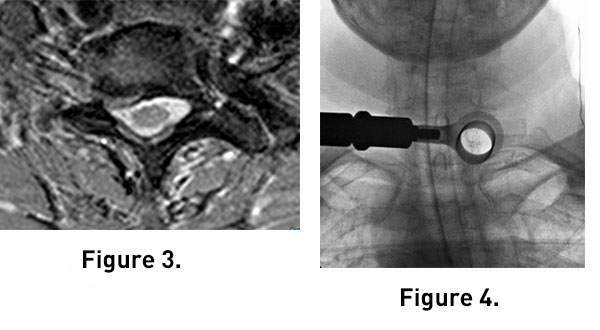
Selected surgical option: Posterior minimally invasive C7-T1 foraminotomy and discectomy (Fig. 4). This approach was chosen to avoid the potentially complicated dissection through a scarred surgical bed and to eliminate the need to fuse another cervical level. The approach was gained through a 16 mm by 60 mm tube and performed using microscopic magnification. After the foraminotomy was performed, sequestered fragment was found lodged between the T1 pedicle and the C8 root and removed.
Outcome
The patient underwent uncomplicated outpatient surgery. Radicular pain immediately resolved. Unfortunately, very little motor or sensory recovery was achieved at 1-year follow up.
Discussion
Adjacent segment degenerative disease after ACDF surgery is relatively common. Symptoms can result from foraminal encroachment of individual roots or central compression of the spinal cord.
Biomechanical studies have demonstrated that hypermobility and increased stress in the adjacent segments to a fused level will influence mechanical properties of intervertebral discs and joints and contribute to degenerative changes.
Cervical spine surgery for adjacent segment disease can be classified as fusion and non-fusion procedures. The more commonly used technique is revision through anterior cervical discectomy and fusion (ACDF). A second option is posterior decompression and fusion. A third option, chosen in this case, is the minimally invasive posterior cervical foraminotomy (PCF). A fourth option is a to consider a cervical total disc arthroplasty. There is little literature comparing these 3 options in this context.
On the one hand, ACDF or arthroplasty in the revision setting is a tedious operation since the exposure of the required surgical field entails dissection through previous scarred tissue. This carries the risk of injury to vital structures of the neck such as the esophagus and the recurrent laryngeal nerve. Furthermore, foraminal disc fragments can sometimes be difficult to safely retrieve when approached through the disc space. The risk of graft subsidence and pseudarthrosis may compromise long-term outcome of any fusion procedure.
On the other hand, PCF can be achieved with a less invasive approach to the neural foramen, allowing for direct decompression of the nerve root, especially for lateral foraminal disc herniations. PCF also obviates the need for fusion, often resulting in faster recovery and decreasing the expense associated with the procedure. However, the same stresses that led to the adjacent disc herniation are still present and possibly enhanced. Thus, there is a risk for additional degenerative disc disease or secondary herniation, and possibly neck pain.
In general, the authors prefer the least invasive option and consider additional surgery if clinically necessary.