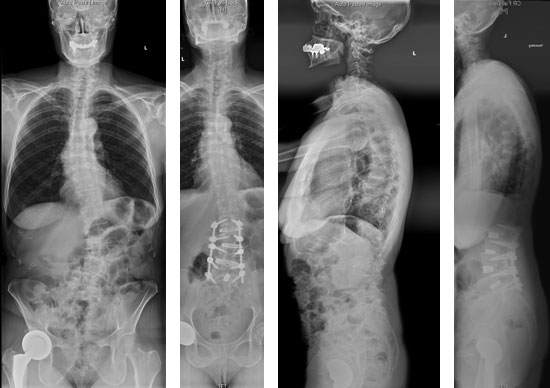
Circumferential Minimally Invasive Surgery (cMIS) for Correction of Degenerative Lumbar Scoliosis
Ibrahim Hussain, MD
Roger Härtl, MD
Age: 69 years old
BMI: 24 kg/m2
Ambulatory Status: Independent
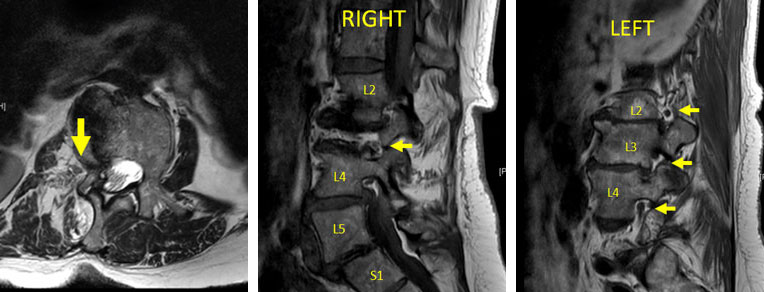
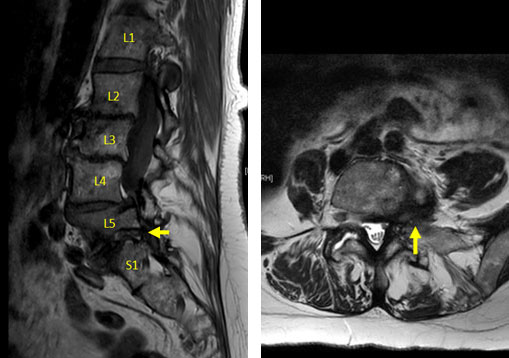
HPI: 68F with PMH R hip and bilateral knee replacements presents with complaints of progressively worsening low back and bilateral leg pain over the past 2 years. Back pain is mechanical in nature, worse with ambulation and changing positions. Radicular symptoms involve the right groin area/upper thigh (L2, L3 distribution), and left lateral aspect of the leg down the front of the shin to the dorsal foot (L5 distribution). Paresthesias in these same regions. No weakness endorsed. R hip and knee etiologies for LE pain excluded by orthopedist. Failed multiple conservative measures during this time period including PT, ESI.
PMH: Afib on Eliquis
PE: Motor 5/5 throughout
Sensation intact to LT/PP throughout
No myelopathy
ODI: 48/100
DEXA: T-score = 0

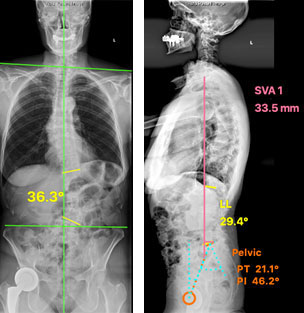

Goals of Surgery: cMIS coronal deformity correction, indirect/direct foraminal decompression
Procedure
1. L2/3, L3/4, L4/5 lateral transpsoas interbody fusion (right side approach)
2. L5/S1 transforaminal interbody fusion (left side approach)
3. L2-S1 percutaneous pedicle screw instrumentation with 3D navigation
Alternative option for L5/S1 level could be standard approach ALIF, lateral approach ALIF, or OLIF
- No prior history of abdominal surgery
- Could achieve bilateral indirect decompression
- Hyperlordotic cage would allow for more segmental lordosis and global lumbar lordosis correction
- With lateral ALIF and OLIF, could perform all interbody work from single lateral position
- However, the most prominent exam/imaging finding was severe left L5 radiculopathy and severe left foraminal stenosis at L5/S1
- Therefore a direct decompression with facetectomy and TLIF was chosen to treat this level to ensure adequate left L5 nerve root decompression

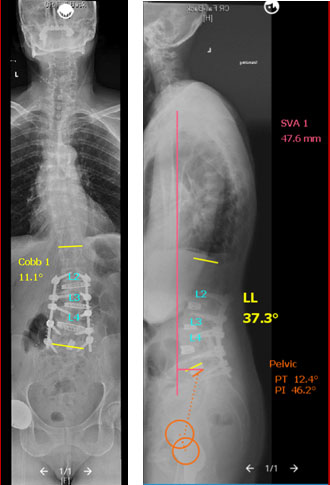
Postoperative Course
- Postop course notable for ileus, resolved in 2 days
- No blood transfusions
- Sensorimotor intact
- Eliquis resumed POD #5
- DC’d home POD #6
- 3-month follow-up – Off narcotics, back to work and normal activity, minimal residual right leg pain. Left leg pain resolved.