- Home
- Circumferential Decompression of Thoracic Spinal Cord via Endoscopic Biportal Transpedicular Corpectomy for Renal Cell Metastases
Circumferential Decompression of Thoracic Spinal Cord via Endoscopic Biportal Transpedicular Corpectomy for Renal Cell Metastases
Yohannes Ghenbot, MD, MS; Jang W Yoon, MD
Department of Neurosurgery, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States
Patient History/Exam
A 71-year-old male with renal cell carcinoma (RCC) and known T12 pathologic compression fracture presented to the emergency room for intractable back pain and symptoms of myelopathy including subjective lower extremity weakness and unsteady gait.
Neurologic exam was notable for full strength in the lower extremities, normal sensation, and preservation of rectal sensation and voluntary rectal contraction.
Pre-operative Imaging
Preoperative imaging included standing XR, CT, and MRI (Figure 1) with and without contrast. Standing radiographs and CT imaging were notable for a lytic T12 pathologic fracture with burst morphology, >50% vertebral body height loss, and 21.7° of focal kyphosis. Contrasted MRI redemonstrated the vertebral body fracture with associated epidural tumor extension ventral to the thecal sac causing Bilsky 3 spinal cord compression.
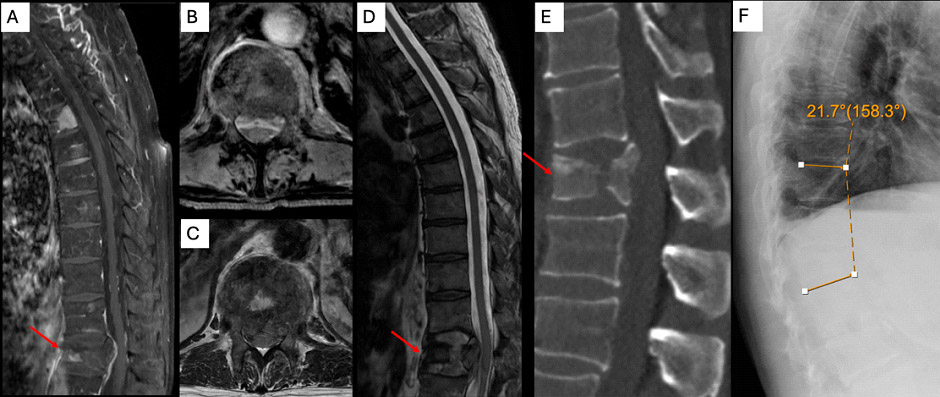
Figure 1: Preoperative imaging. Post-contrast MRI showed multifocal metastasis along the spinal column with associated pathologic compression fracture at T12 (1a & 1b). T2 MRI showed complete effacement of the thecal sac from retropulsed bone and ventral epidural tumor (1c & 1d). Non-contrast CT showed burst fracture morphology (1e). Upright thoracic XRs revealed 21.7° focal kyphosis at the level of the fracture
Diagnosis
The patient’s preoperative symptoms and radiographic imaging were consistent with spinal column instability and spinal cord compression from pathologic burst fracture and epidural tumor.
The patient’s spinal instability neoplastic score (SINS) was 14 as the patient presented with mechanical back pain (3), and imaging showed that the lytic lesion (2) located in the semirigid spine (1) with posterior spinal element involvement (3) resulted in >50% vertebral height loss (3) with 22.1° focal kyphosis (2)
Treatment
Goals:
⦁ Stabilization of unstable T12 pathologic burst fracture through thoracolumbar fusion
⦁ Thoracic spinal cord decompression
Selected surgical procedure – the surgical technique chosen was navigated, percutaneous T9-L3 instrumentation for spinal column stabilization and biportal fully endoscopic corpectomy for spinal cord decompression. This minimally invasive (MIS) technique was chosen over open surgery for several reasons. First, an MIS approach can hasten time to radiation as MIS spinal surgery involves less tissue disruption. Second, patients with metastatic disease are frequently in fragile states with limited life expectancy. An MIS approach has the potential to maximize time outside of the hospital and rehabilitation facilities through reduced wound complications and length of stay.
Spinal column stabilization – first, a small midline incision was made over the L1 spinous process for placement of a spinous process clamp. An o-arm scan was performed for navigation. Pedicle screws were placed from T9-L3 using a navigated drill guide, screw, and k-wire. The level of the fracture was not instrumented in anticipation of corpectomy. A post-instrumentation o-arm scan confirmed accurate placement of pedicle screws.
Spinal cord decompression – an incision was made at the left T12 pedicle and the left T11 pedicle for passing of surgical instruments and the endoscopic camera, respectively. Hemostasis was obtained through a radiofrequency ablator. First, the dorsolateral spinal cord was decompressed. An osteotome was used to remove the facet and gain access to the pedicle while a 5.5mm drill and Kerrison rongeurs were used to remove the lamina and spinous process. Next, the vertebral body was accessed through the left T12 pedicle and corpectomy was performed using a combination of down-pushing curettes, straight pituitaries, and curved pituitaries (Figure 2). Adequate decompression was assessed with the endoscopic camera and the spinal cord was found to be pulsating. After achieving hemostasis, a hemovac drain was placed in the cavity. Finally, a rod was passed through pedicle screw extension tulips and final tightened. The region of the fracture was decorticated bluntly using a cob and allograft was placed.
Outcome
The patient recovered well in the immediate post operative period. Pathology was consistent with RCC. Postoperative upright XRs showed correction of focal kyphosis (22.1° preoperatively, 11.3° postoperatively, Figure 2). The patient was given clearance for radiation as early as postoperative day 3 and discharged home on post operative day 4. Unfortunately, the patient’s radiation was delayed until 4 weeks after surgery due to hospitalization for metabolic kidney issues.
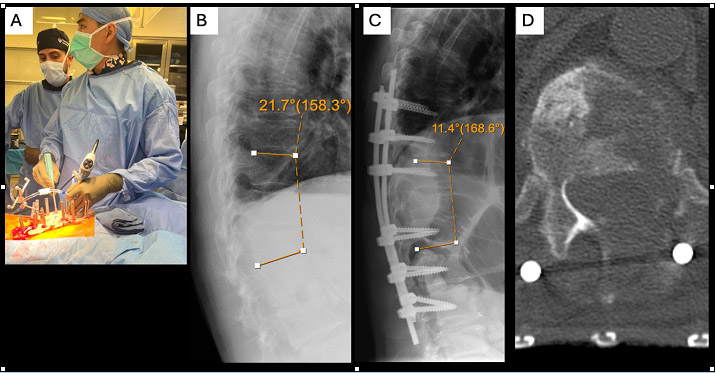
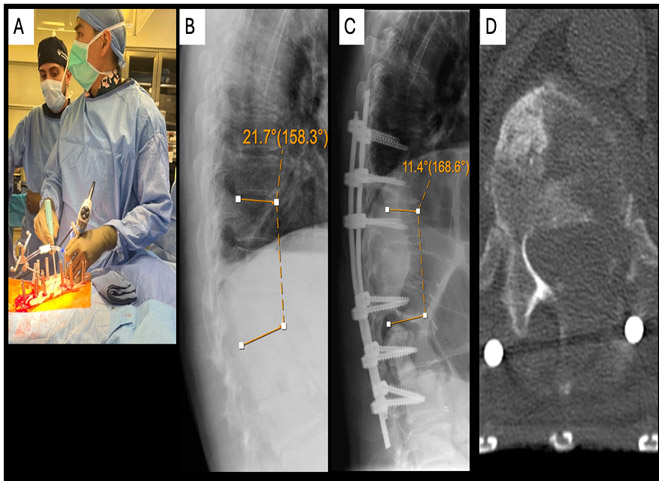
Figure 2: Intraoperative picture and post-operative imaging. Biportal technique allowed for use of standard instruments such as the down-pushing curette (2a). Focal kyphosis associated with the pathologic compression fracture improved from 21.7° preoperatively (2b) to 11.4° postoperatively (2c). Axial CT demonstrated transpedicular corpectomy through the left T12 pedicle (1d)
Discussion
Separation surgery in spinal metastatic disease is largely palliative. Instrumentation of the spinal column improves pain from spinal instability, while circumferential spinal cord decompression preserves ambulatory function.
Patients with spinal metastatic disease are often frail and may not tolerate open surgery, especially when more invasive techniques such as corpectomy are required. Furthermore, increased tissue disruption may lead to more wound complications compared to MIS techniques, which delays postoperative treatment for local and systemic disease control (i.e. radiation and chemotherapy, respectively). MIS approaches also hold promise in reducing length of stay and readmission/reoperation for wound issues. This is especially important in patients with metastatic disease who have limited life expectancy as maximizing time spent outside of the hospital is important.
Prior reports of endoscopic separation surgery largely include patients with purely epidural soft tissue disease. Fully endoscopic partial corpectomy using biportal technique for separation surgery has not been reported in the literature to our knowledge. Endoscopic indications will continue to expand with advancement in technology and technique adoption by spine surgeons.