- Home
- Endoscopic Posterior Cervical Foraminotomy for C3 Radiculopathy
Endoscopic Posterior Cervical Foraminotomy for C3 Radiculopathy
Peter B. Derman, MD, MBA
Texas Back Institute Dallas, Texas, USA
Patient History / Exam
A 64-year-old male truck driver presented to the outpatient clinic with one week of acute onset left-sided upper cervical discomfort radiating to the left occiput, behind the left ear, and to the left temple. He also experienced numbness in the left anterior neck and jawline. He was unable to work due to the severity of his pain, which he rated at 8 out of 10 in intensity. No other symptoms were present. He initially presented to an emergency department, where stroke workup was negative.
On physical exam, he was visibly uncomfortable due to pain. There was diminished sensation to light touch in the left anterior neck and jawline. Spurling’s sign was positive on the left, which exacerbatedthe pain radiating from the left upper neck to the left temple. Strength and sensation were intact in the bilateral upper and lower extremities, and there were no pathologic reflexes or hyperreflexia.
Pre-Operative Imaging

Figure 1. Upright AP, lateral, and lateral flexion-extension radiographs of the cervical spine demonstrated straightening of the sagittal contour with anterior osteophytes at multiple levels. There was no spondylolisthesis or instability.
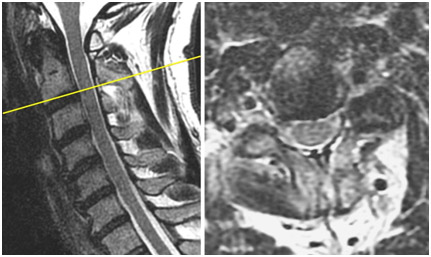
Figure 2. Non-contrast MRI of the cervical spine revealed severe left foraminal stenosis due to spondylosis at C2-3. There was also bilateral foraminal stenosis at C4-5 and C5-6 but no significant canal stenosis throughout.
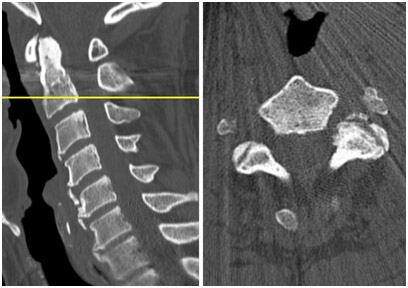
Figure 3. Non-contrast CT of the cervical spine demonstrated osseous foraminal stenosis most severe on the left at C2-3.
Diagnosis
Left C3 radiculopathy stemming from left C2-3 foraminal stenosis due to spondylosis.
Treatment
The patient’s symptoms persisted for months despite physical therapy, non-steroidal anti-inflammatory medications, a weeklong course of oral steroids, muscle relaxers, and gabapentin. He obtained no relief, even transiently, from a left C3 selective nerve root block. The decision was made to proceed with surgical decompression. He underwent an outpatient uniportal endoscopic posterior cervical foraminotomy without complication.
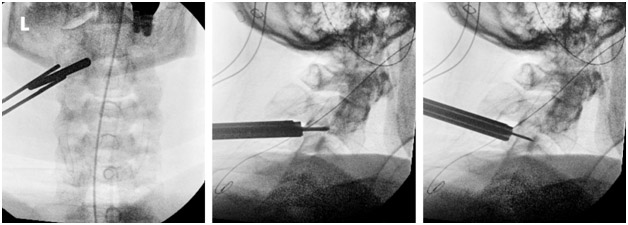
Figure 4. Intra-operative AP fluoroscopy image demonstrating localization and docking over the left C2-3 neuroforamen. Lateral images at the conclusion of the procedure confirming decompression from the caudal aspect of the C2 pedicle to the cranial aspect of the C3 pedicle.
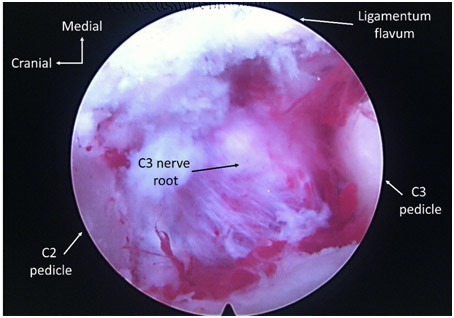
Figure 5. Photograph taken through the endoscope illustrating the unroofed left C2-3 neuroforamen with decompressed C3 nerve root.
Outcome
The patient experienced immediate and dramatic improvement in his symptoms. He took no pain medication whatsoever after surgery and was rapidly back at work. Athis six-week post-operative visit, he had complete resolution of his pain. Sensory symptoms were significantly better and continuing to improve. He is now nearly a year out from surgery and still doing well.

Figure 6. Photograph of well-healed surgical incision six weeks after surgery.
Discussion
Upper cervical radiculopathy is a relatively infrequent diagnosis that may be underappreciated even when present. If patients remain symptomatic despite conservative measures, surgical intervention can be beneficial. Endoscopic posterior cervical foraminotomy is an ultra-minimally invasive, motion-sparing, non-instrumented procedure that can effectively treat this condition without the approach-related complications associated with anterior surgery in the upper cervical spine (e.g., dysphonia and dysphagia).