- Home
- Percutaneous Headless Compression Screw Fixation with Endoscopic Debridement and Bone Grafting of Bilateral Chronic L5 Pars Fractures
Percutaneous Headless Compression Screw Fixation with Endoscopic Debridement and Bone Grafting of Bilateral Chronic L5 Pars Fractures
Christopher A. Yeung, MD
Desert Institute for Spine Care, Phoenix, AZ, USA
Patient History / Exam
A 15 year 1 month old male high school wrestler presented with a 5 month history of low back pain without radicular symptoms after climbing a rope and falling 15 feet and landing on his feet. He was diagnosed with bilateral L5 pars fractures with x-ray, MRI, and CT. He had been treated with rest and bracing for 11 weeks and his pain decreased, but a repeat CT scan just before this referral showed persistent bilateral pars fractures. Pain ranged from 1-7 out of 10.
Further nonoperative treatment for 3 months included a bone stimulator and physical therapy with neutral spine stabilization exercises. His pain completely resolved during this time. Repeat CT scan at 8 months post injury however revealed persistent bilateral L5 pars fractures. Since he was asymptomatic he was cleared to gradually return to sporting activities.
He had recurrent back pain that waxed and waned for years and was managed by activity modification. He started training to become a firefighter and his back pain symptoms became unbearable again. He returned to the clinic now as a 19-year 8-month-old.
On physical exam, he had pain with range of motion especially extension. He had positive stork signs. He was neurologically intact with full motor strength, sensation, and 2+ reflexes.
Pre-Operative Imaging

Figure 1. Upright lateral flexion-extension radiographs of the lumbar spine demonstrated bilateral L5 pars fractures without spondylolisthesis.

Figure 2. CT scan 4 years post injury demonstrated persistent chronic bilateral L5 pars fractures with some widening of the fracture sites and more sclerotic margins compared to his earlier CT scans. This is classified as Terminal stage lesions (rather than Early or Progressive lesions) and a fracture nonunion. From left to right, axial view, left sagittal pars view, right sagittal pars view.
Diagnosis
Bilateral L5 chronic pars fractures with nonunion over 4 years post injury
Treatment
The patient’s back pain limited his strenuous physical activity and he was training to for a career as a firefighter which is a profession that requires intense physical activity. I recommended a bilateral pars fracture repair with endoscopic fracture debridement and bone grafting with demineralized cortical fiber allograft bone and fixation with percutaneous headless compression screws.
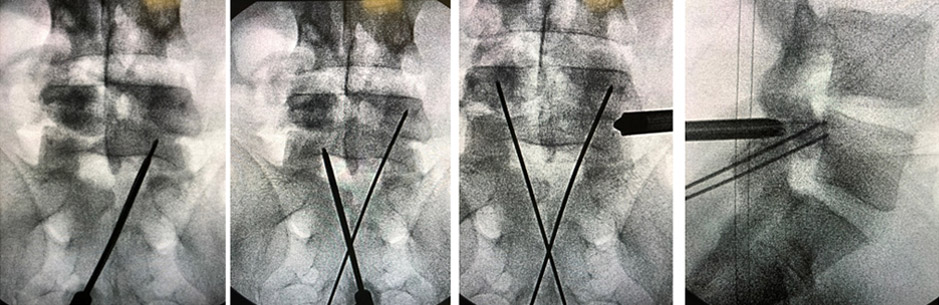
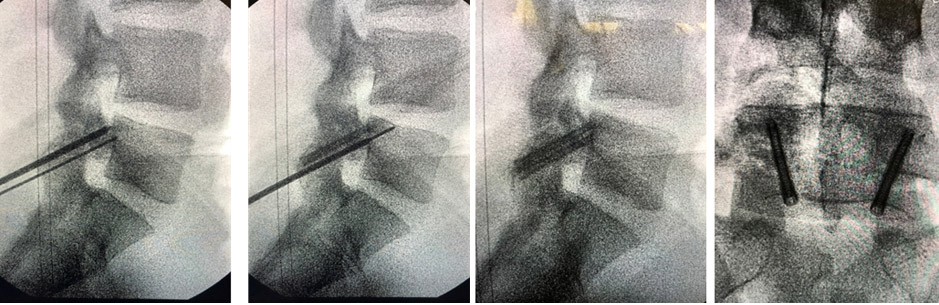
Figure 3. Intraoperative flouroscopic images demonstrating a Jamshidi needle to start the trajectory to cross the pars fractures and then passing a K-wire through the Jamshidi needle across the pars fractures. I then performed endoscopic debridement and bone grafting with 2 cc of demineralized cortical fibers through the working channel of the endoscope. After applying the bone graft I used a cannulated tap and placed 34 mm and 36 mm long 5.0 mm headless compression screws for secure fixation. I have since modified my technique to pass the K wire just short of the fracture site and then perform the endoscopic debridement and bone grafting. After the bone grafting I will then pass the K wire across the fracture site and then tap and place the screws.
Outcome
The patient experienced rapid and dramatic improvement in his symptoms. He was essentially asymptomatic at his 2-week postop visit rating his pain at 0-1 out of 10. This pain-free state continued up to his last follow-up visit at 1 year postop. His postoperative precautions included 6 weeks of bracing with an LSO. At 2 weeks postop he returned to work was advised to avoid excessive bending, twisting, and lifting more than 15 pounds. At 2 months postop he had resumed neutral spine trunk stabilization exercises and was advised to avoid strenuous activities but could otherwise use his pain level as a guide to what he could and could not do. At 6 months postop CT scan revealed solid bony union and he was cleared for unrestricted activities. He was last seen at 1 year postop for x-rays and he was asymptomatic. He is now 2 years postop.

Figure 4. Postoperative imaging 6 months after surgery shows solid fixation on x-rays and the axial and sagittal CT scan images show the pars fractures are completely healed with solid bony union.
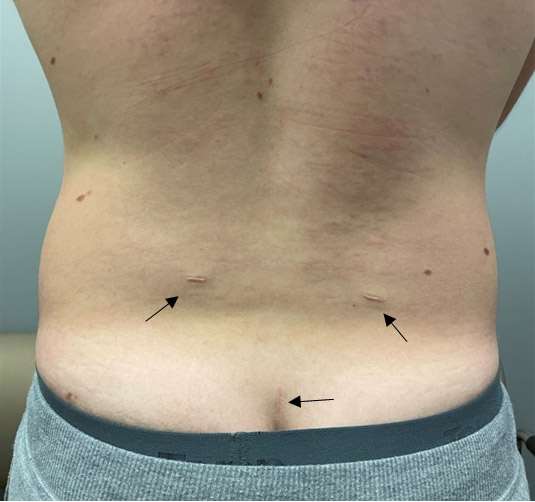
Figure 5. Photograph of 3 well-healed surgical incisions. He had 2 paraspinal incisions for the endoscopic debridement and 1 midline stab incision for the percutaneous screws.
Discussion
Pars fractures are common in adolescent athletes. Many of these heal with nonoperative treatment and bracing especially if diagnosed early as an acute fracture, but nonoperative treatment can be long and frustrating with recurrent symptomsand a relatively high rate of chronic pars fracture nonunions.
Literature suggests nonoperative treatment for at least 6 months before offering operative treatment, likely due to the relatively invasive historical surgical treatment options. In 1970 Buck described direct fracture fixation with a 4.5 cortical screw with open debridement and iliac crest bone grafting. Levi has described a modified Bucks Technique using percutaneous fully-threaded cortical screw direct fixation with MIS tubular debridement and bone morphogenic protein (BMP). This resulted in successful fracture healing in 20 out of 21 patients.
Cannulated headless compression screws represent a technological advancement to easily achieve both secure fixation and compression across the fracture site without any prominent hardware compared to a lag screw (or over drilling proximally with a fully threaded cortical screw) which only has proximal fracture fixation with the head of the screw. A fully-threaded cortical screw provides secure fixation across the fracture site, but lacks compression across the fracture site.
Most often I utilize this technique without the need for direct fracture debridement and bone grafting. This is especially true with pars fractures in the early or progressive lesion stage on CT scan along with a high signal change on T2 and/or IR/STIR MRI scans. If bone grafting is desired, endoscopic surgery for debridement and application of bone grafting is ultra-minimally invasive and effective. The approach trajectory is from a posterolateral approach similar to the approach angle targeting an extraforaminal herniation (about 4-7cm lateral from the midline. The initial needle placement can confirm targeting of the pars fracture with an injection of contrast dye to outline the fracture site. The fracture site is prepared first with a bipolar radiofrequency probe to remove soft tissue and achieve hemostasis. Then an endoscopic burr is used to debride the fracture site. When applying the bone graft, the endoscope is optimally positioned relative to the fracture, the irrigation is turned off, and the graft is placed through the working channel of the endoscope. It is debatable whether it is best to use iliac crest bone graft, BMP, or demineralized bone matrix(DBM). I had a detailed discussion with the patient and parents about this and together with shared decision making they opted for the DBM.
Direct pars fracture repair can now be accomplished in a minimally invasive, percutaneous surgery and does not adversely affect the target motion segment nor any adjacent motion segments. Pars fracture nonunionare common and can result in spondylolisthesis later in life which may necessitate a lumbar fusion. Surgically fixing these fractures can prevent the need for future fusion and does not adversely affect adjacent levels. I suggest consideration for offering this percutaneous headless screw surgical technique prior to failing 6 months of nonoperative treatment. Acute pars fractures would have a higher and faster healing rate and would not need direct debridement and bone grafting compared to chronic fractures.
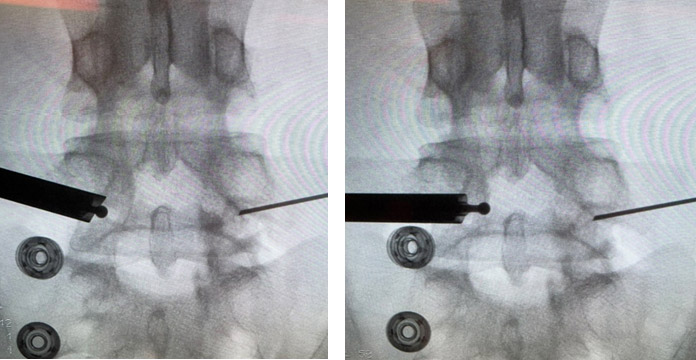
Figure 6. A different case with PA fluoroscopy images demonstrating initial spinal needle placement into the pars fractures verified with injection of contrast dye to outline the fractures. On the rightside some of the contrast leaks into the epidural space after increasing the volume injected. The drill is used to debride the fracture site under direct endoscopic vision and spot checks with fluoroscopy can confirm debridement across the entire fracture. The drill is used on the left pars fracture here.
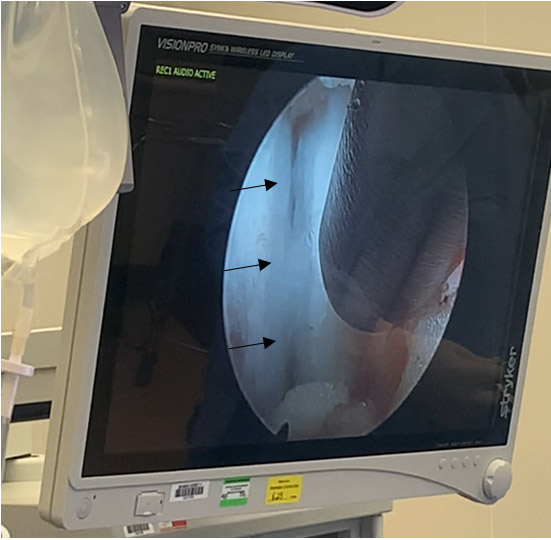
Figure 7. A different case showing the endoscopic view of a chronic pars fracture after clearing the soft tissue off with the RF bipolar probe and before debriding with the drill.