Extraforaminal L5-S1 Left Lumbar Side Herniation Causing Severe L5 Radiculopathy. Extraforaminal Minimally Invasive Microdiscectomy with 3D Navigation and Intraoperative CT Guidance
Miguel A Roldán Serrano, MD
Raj Nangunoori, MD; Roger Härtl, MD
Weill Cornell Brain and Spine Center. New York, NY (USA).
History
The patient was a 76 year-old-male who was referred for an evaluation by his neurologist after progressively worsening “lancinating” left leg pain on the lateral aspect of the left thigh into the lateral knee. He also noted subjective walking impairment due to his symptoms. For the last several months, the patient had attempted conservative measures including physical therapy and medications with no significant lasting relief. Denied any low back pain, weakness, right leg symptoms, or urinary or bowel issues.
Examination
The patient was neurologically intact with no obvious motor weakness, but with a positive Lasegue’s sign on the left and negative FABER. Sensory exam was suggestive of hypoesthesia along the left L5 dermatome.
Imaging
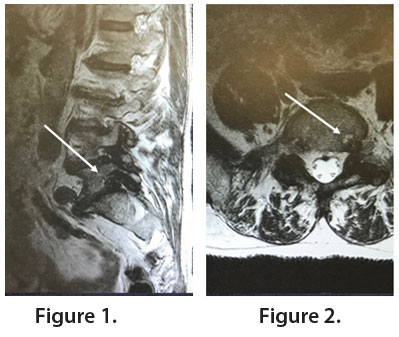
MRI T2-weighted sagittal (Figure 1) and axial (Figure 2) demonstrated the presence of a foraminal disc herniation at the L5-S1 level causing severe compression of the exiting left L5 nerve root.
Diagnosis
Left L5 radiculopathy secondary to foraminal-extraforaminal left L5-S1 lumbar disc herniation
Treatment
Goal: Decompression of the affected left L5 nerve.
Challenge: Compared with the paramedian approach, the far lateral “outside-in” approach utilizes a corridor that may be unfamiliar to many surgeons. The challenge with this approach is appropriate localization and identification of the relevant anatomy including the transverse process, facet joint, pars, and pedicle of the nerve root that is compressed. Understanding the anatomy is essential in preventing iatrogenic nerve injury and to prevent excessive nerve manipulation, which can lead to postoperative dysesthetic pain and motor dysfunction. In addition, working through a minimally invasive corridor with tubular retractors has a significant learning curve.
Surgical Plan: Far lateral minimally invasive discectomy with 3D navigation
Surgical Procedure: Due to the challenging working corridor, coupled with the level of the pathology in this case, 3-D image guidance with navigation was used. Images were obtained with an intraoperative CT scanner (Airo, BrainLab, Munich, Germany).
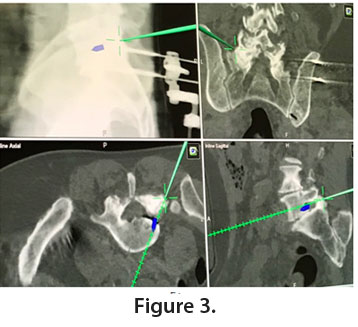
The patient is positioned in prone and draped on a Jackson table and a navigational reference array is anchored to the iliac crest. An intraoperative CT scan is obtained and downloaded to the navigation work station, enabling use of the stereotactic pointer. The pointer is used to identify the entry point on the skin and the optimal trajectory to reach the lateral aspect of the neural foramen. After a skin and fascial incision is made, the pointer is used to confirm an appropriate docking surface. A series of sequential dilators is used until a 15-mm diameter tubular retractor is positioned and anchored to the table. Once the tubular retractor is in place, the pointer is again used to confirm the anatomy. A small “virtual” screw (blue, Figure 3) can be digitally placed as a target to represent the disc herniation of interest.
Muscle is detached with monopolar cauterization to expose bony structures (Figure 4). High-speed drilling is performed to enlarge the diameter of the foramen, identify the pedicle and the exiting root (Figure 5). Care should be taken to remove minimal bone necessary from the facet to prevent instability.
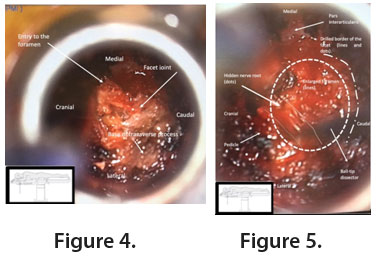
When identified, the nerve is mobilized (preferably cranial and medial) from the herniation (Figure 6) which is finally incised and removed. Adequate decompression of the nerve is checked with ball-tip dissectors. Finally, appropriate hemostasis is ensured before closing and removal of the retractor.

Outcome
Postoperatively, the patient ambulated the same evening and remained in the hospital overnight. He was discharged home with resolution of his symptoms the next morning. At follow-up, he was neurologically intact, pain-free and had resumed working.
Discussion
The far lateral (extraforaminal) approach has been described and largely used for several years to manage foraminal and extraforaminal lumbar disc herniations. Advantages include decreased muscle trauma and less bony removal which prevents iatrogenic instability. Importantly, the far lateral approach facilitates the decompression of the exiting nerve without needing a fusion based on the anatomic location of the disc herniation. The most common involved level is L4-L5, however can occur at other levels, as in the illustrated case. The L5-S1 level can be particularly challenging due to the iliac crest. Thus, 3D navigation using intraoperative CT image guidance is ideal for finding the optimal trajectory to the foramen while avoiding the iliac crest.
Using navigation, the skin and fascial incisions could be planned, and the tubular retractor could be checked to ensure it was over the anatomical region of interest. In the illustrated case, hypertrophied and/or sclerotic facet joints can obscure normal anatomy. With intraoperative navigation, the starting point for bony drilling can be identified, and amount of bone removal can be minimized to prevent instability. Navigation can also be used to confirm the pedicle position of the exiting nerve root and prevent unnecessary manipulation of the nerve. Additionally, the use of navigation obviates the need for fluoroscopy, reducing radiation exposure to the surgical team.
References:
-
- H Soliman, JFA Telfeian, DB Choi, M Galgano, T Kosztowski, ZL Gokaslan, AA Oyelese. Minimally invasive, far lateral lumbar microdiscectomy with intraoperative computed tomography navigational assistance and electrophysiological monitoring. World Neurosurg. 2019; 122: 1228-1239.
- Siu TL, Lin K. Microscopic tubular discectomy for far lateral lumbar disc herniation. J Clin Neurosci. 2016; 33:129-133.