Lumbar Tubular Decompression Through An Interspinous Midline Approach With Microscopic Assistance
Nicolas Coombes, MD
Cristian Fuster, MD
Axial Medical Group,
Buenos Aires Argentina
History:
76-year-old man with medical records of hypertension, with no history of previous spinal surgery.
History of 2 years of progressively worsening pain and dysesthesia in both anterior quadriceps, distribution of L2 and L3 territory above the knees, neurological claudication, and inability to walk no more than 50 Mts. No low back pain, history of several epidural blocks (L2/L3 level) performed under CT with a good response.
Examination:
After his physical examination, we observed that he had a normal motor function, dysesthesia in L2 and L3 territory, above the knees that did not extend to the leg.
Valsalvaand Wasserman maneuverwere positive.
Pre-Operative Imaging:
The X-ray images show a correct sagittal and coronal balance. (Figure 1 -2)
In the MRI images, multilevel degenerative pathology with severe central stenosis at the L2 /L3 level is observed (see Fig. 3-4-5)
Figures
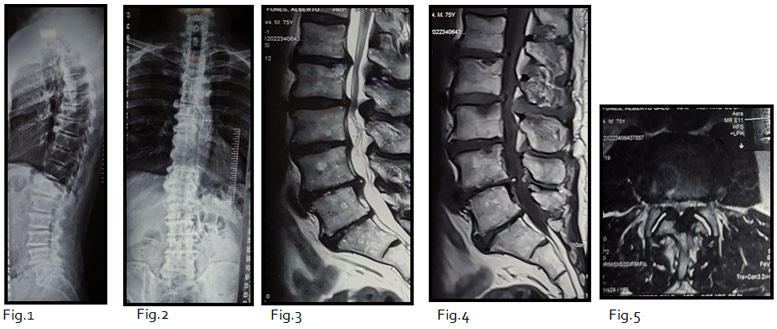
Fig1 and 2. Full X-ray with a good coronal and sagittal balance. Fig 3 to 5. MRI T2 and T1 weighted showing in sagittal and axial view central stenosis at L2 level with flavum ligament hypertrophy and central hypertrophy facet joints.
Diagnosis :
76 y/o male with Lumbar central stenosis at L2
Treatment
The objective of the treatment is to achieve a wide central decompression and both roots decompression.
Challenges
Preserving facet joints on both sides to avoid instability.
The surgical procedure that we choose was a midline tubular interspinous approach
with microscope assistance
Outcome:
Intraoperative
We use an 18 mm tube which is introduced gradually between 2 interspinous process (L2-L3) the upper segment of the spinous apophysis is drilled, as suggested in the literature1
(Fig. 6-7-8)
Once in the midline, the yellow ligament is removed, and the tube is advanced to both sides as much as necessary for root decompression on both sides.
The central position through which the tube enters allows it to be angled to both sides equally allowing root decompression to be equally on both sides. (Fig. 9 ,10,11,12)
The operating time was 118 min, obtaining a good central and bilateral decompression.
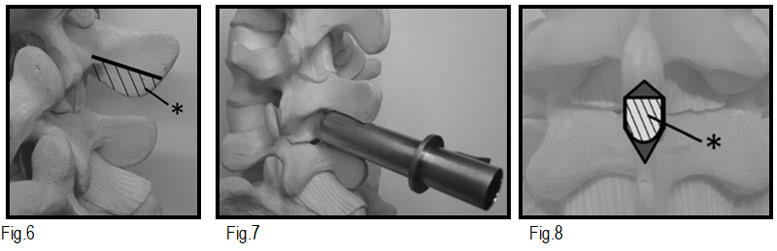
Fig 6,7,and 8 Placing the tubular retractor. The approach is from the midline incision in the supra- and interspinous ligaments and periosteum of the spinous process, so no muscular tissue is seen on the field of view from: Mikami Y, Nagae M, Ikeda T, Tonomura H, Fujiwara H, Kubo T. Tubular surgery with the assistance of endoscopic surgery via midline approach for lumbar spinal canal stenosis: a technical note. Eur Spine J. 2013;22(9):2105-2112. doi:10.1007/s00586-013-2806-5
Postoperative:
At 2 hours post-surgery he began to mobilize, being discharged the 8 hours of postoperative. He currently has an 18-month pain-free follow-up.
Postoperative Images:
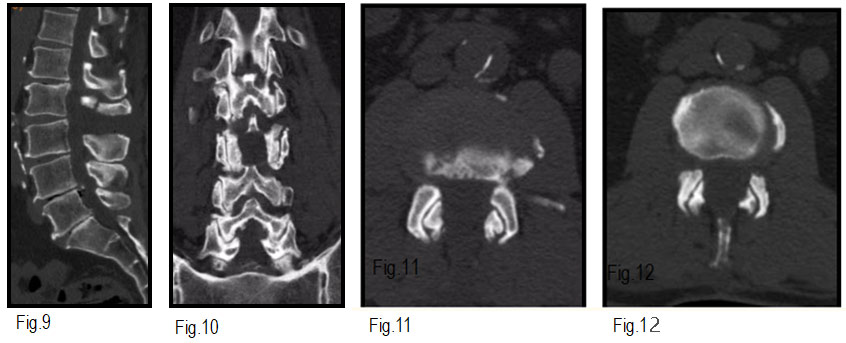
Fig. 9 to 12. Facet joint preservation. The tubular retractor is tilted to both sides, decompression is performed while preserving the facet joints.
Follow-up images: a wide central decompression is observed, compared to the
preoparatory images with improvement of the symptoms without their reappearance.
Fig 13 to 15
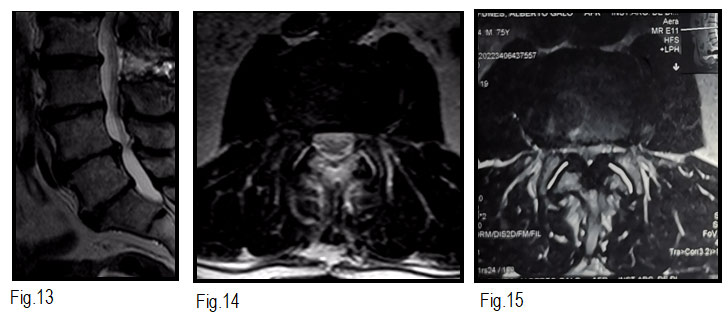
Fig. 13 to 15. MRI T2 weighted sagittal and axial view with a wide central decompression preserving booth facets joint.
Discussion:
In cases of central stenosis and symptoms of bilateral radiculopathy, decompression on the side of the paramedian approach may be insufficient. When a paramedian approach is selected for patients with narrow lamina width or the superior lumbar spine, preservation of the inferior articular process of the superior lumbar spine may become difficult.1
If bone excision is minimized to preserve facet joints on the approach side, decompression may not be sufficient, or the working space may become small. Until the surgeon becomes skilled at tubular surgery, peeling the dura and ligamentum flavum and performing decompression in a narrow working space is difficult.
With this method, where a medial incision is made to the supra and interspinous ligaments and the periosteum of the spinous process, direct damage is not caused because muscle tissue is not present in the operative field.
Partial resection of the superior spinous process for midline access will avoid paramedian muscle dissection and would provide the possibility of preserving both joints, allowing decompression to be more effective bilaterally.
A biomechanical study reported instability following detachment of the supraspinous ligament whereas another researcher reported that resection of the interspinous ligament did not impair stability of the lumbar spine.23
Although a part of the spinous process and deep layer of the interspinous ligament are resected with this method, a shallow layer and the supraspinous ligament can be constructed by retaining sufficient tension. Instability was not observed in this patient 18 months after surgery, but the impact of this approach on spinal stability has not been clarified. This is a limitation of our method and further long-term observation is necessary.1
Bibliografy:
- Mikami Y, Nagae M, Ikeda T, Tonomura H, Fujiwara H, Kubo T. Tubular surgery with the assistance of endoscopic surgery via midline approach for lumbar spinal canal stenosis: a technical note. EurSpine J. 2013;22(9):2105-2112. doi:10.1007/s00586-013-2806-5
- Tai CL, Hsieh PH, Chen WP, et al. Biomechanical comparison of lumbar spine instability between laminectomy and bilateral laminotomy for spinal stenosis syndrome—an experimental study in porcine model. BMC MusculoskeletDisord. 2008;9:88. doi: 10.1186/1471-2474-9-84.
- Hartmann F, Janssen C, Böhm S, et al. Biomechanical effect of graded minimal-invasive decompression procedures on lumbar spinal stability. Arch Orthop Trauma Surg. 2012;132:1233–1239. doi: 10.1007/s00402-012-1543-2.