Radiculopathy in the Setting of Multilevel Stenosis and Auto Fused Grade 2 Lytic L5-S1 Spondylolisthesis
Peter Derman, MD, MBA
Texas Back Institute
Patient History / Exam:
A 75-year-old male with a history of years of intermittent, tolerable axial low back pain presented with two months of severe low back and lower extremity pain that was worse with bending forward. He described pain in his low back that radiated to the bilateral buttocks and down the left greater than right lower extremity in a distribution most consistent with L4. The lower extremity symptoms were worse than the low back pain, but both were significant. He was essentially wheelchair-bound on presentation. On exam, he had difficulty ambulating due to pain. He was neurologically intact with the exception of 4/5 strength in the left extensor hallucis longus and bilateral tibialis anterior.
Pre-Operative Imaging:

Figure 1: Upright AP and lateral radiographs of the lumbar spine demonstrating grade 3 L5-S1 lytic spondylolisthesis. There was no instability on flexion-extension views.
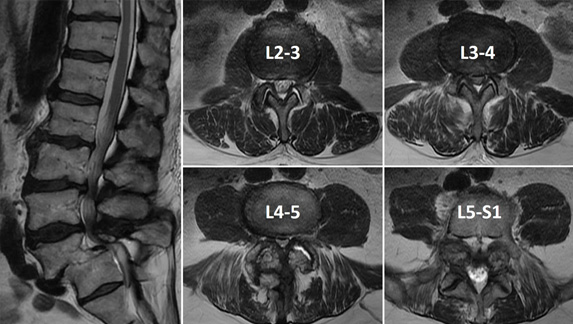
Figure 2: Mid-sagittal and select axial T2-weighted MRI cuts demonstrating spondylosis causing severe pan-stenosis at L3-4 and L4-5. The L5-S1 grade 3 lytic spondylolisthesis is visualized.
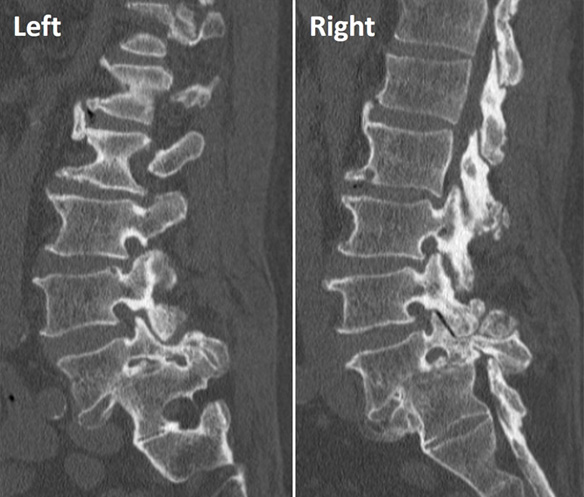
Figure 3: Left and right para-sagittal CT cuts demonstrating in situ autofusion at L5-S1 with severe bilateral foraminal stenosis.
Diagnosis:
Lumbar radiculopathy (primarily bilateral L4 distribution) in the setting of spondylosis causing severe L3-4 and L4-5 pan-stenosis above an L5-S1 grade 3 lytic spondylolisthesis that had autofused in situ.
Treatment:
Given the acute nature of his symptoms, the L3-4 and L4-5 levels (rather than the autofused L5-S1) were felt to be responsible. The decision was made to move forward with surgical decompression of these levels with the understanding that additional, and likely more complex, surgery may be necessary to address L5-S1 if he obtained inadequate relief from the proposed operation.
The patient underwent an uncomplicated L3-4 and L4-5 decompression (unilateral left-sided hemilaminotomies for bilateral decompression) using tubular retractors. Estimated blood loss was 10 cc. He was discharged home 2.5 hours after the conclusion of the procedure.
Outcome:
The patient experienced complete resolution of his bilateral lower extremity symptoms nearly immediately after surgery. By the two-week post-operative visit, he had no back pain or lower extremity symptoms whatsoever, and he had complete normalization of his neurologic exam. He remained completely asymptomatic at most recent follow up, one year after surgery.
Discussion:
Minimally invasive spine surgery is as much a philosophy as a set of techniques. Surgeons should combine information gleaned from the history, physical exam, imaging studies, and other tests when relevant to narrow down the source of patients’ symptoms as much as possible. If non-operative measures fail, a targeted procedure can be planned using the least invasive means available. In the case presented, the patient’s symptoms resolved completely after an L3-4 and L4-5 outpatient tubular decompression without the need to address what at first glance appeared to be significant pathology at L5-S1. This obviated the need for a larger and more complex procedure.