Robotic Assisted Minimally Invasive Treatment of Degenerative Kyphoscoliosis
Greg Poulter, MD
HPI/Exam
60 year old female with no significant past medical history presented with chronic and worsening back pain with an inability to stand upright. She noted a slowly progressive spinal deformity with discomfort, poor standing/walking tolerance and rib/pelvis pain. She failed an extensive course of nonsurgical care including injections, therapy and medications. Her physical examination demonstrated a kyphoscoliosis with both sagittal and coronal deformities.
Imaging
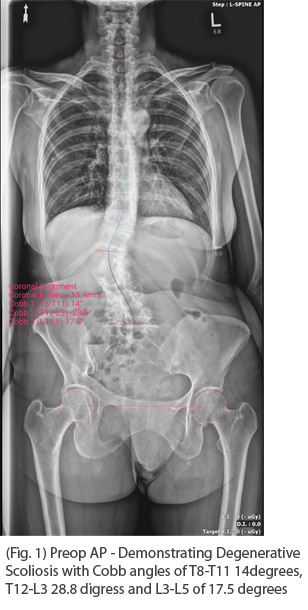
Standing PA and Lateral Scoliosis X-rays demonstrated a 29 degree T12-L3 scoliosis, 65 degree thoracolumbar kyphosis resulting in a 10 cm SVA.
Diagnosis
Degenerative Kyphoscoliosis with sagittal imbalance.
Treatment
Goal: Restore spinal alignment, achieve solid arthorodesis and avoid complications.
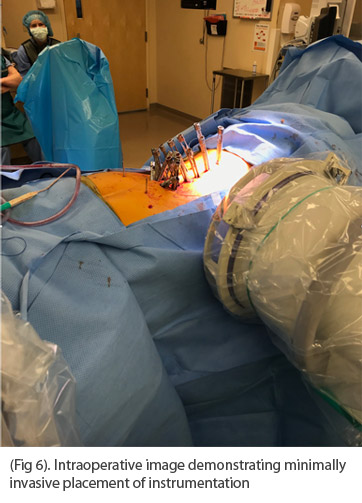
Challenges: Achieve deformity correction with percutaneous techniques, subfascial placement of the rod.
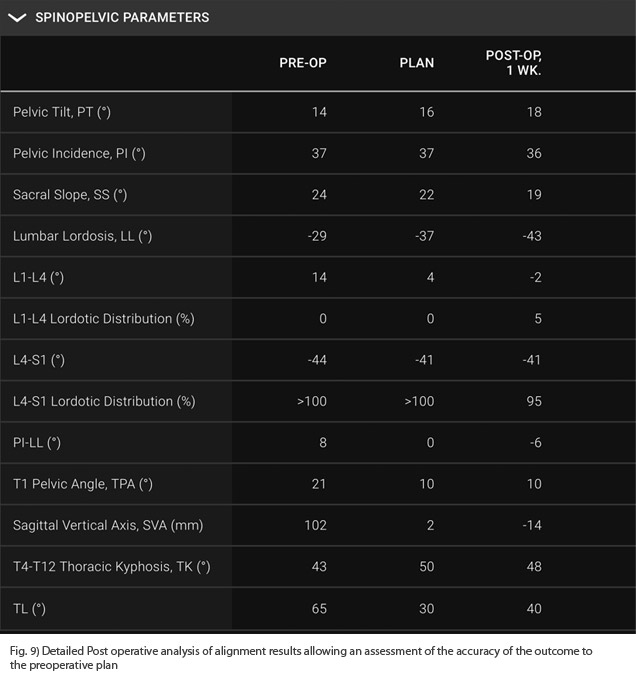
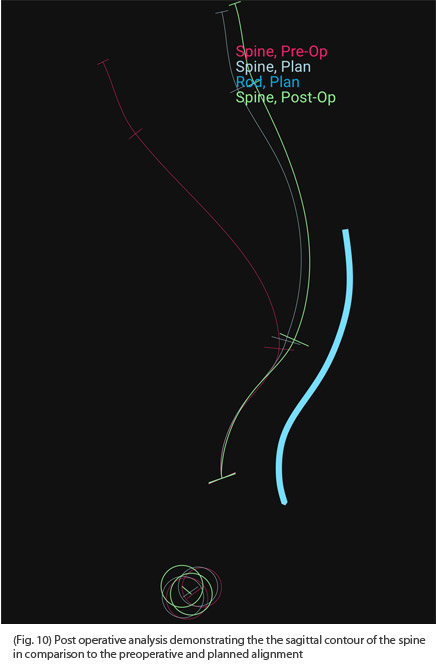
Selected Surgical Option: Prior to surgery, the patient’s desired alignment was modeled both within the Mazor robotics platform software and with Unid platform for the patient specific rods utilizes artificial intelligence algorithms to predict the correction of the pelvic tilt, SVA and thoracic curve above the fusion. Correction of alignment, screw cadence and rod contour were all taken into account to allow a sub facial rod placement that would restore alignment.
The procedure began with an anterior to psoas approach to L2-S1 for four levels of interbody fusion. The patient was then repositioned prone and instrumentation was placed percutaneously with robotic assistance T9-S1 with S2AI fixation. A posterior fusion was performed T9-L2 by decorticating the spine thought stab incisions and placing bone graft and biologics along the lamina. Pedicle screws that with significant reduction forces were augmented with cement. Once provisionally reduced to the rod by tightening the set screws, final coronal adjustments were made by compression and distraction prior to final tightening. The patient had and EBL of 200cc and was discharged home without complications on POD #4.
Postoperative analysis of her X-rays gave detailed information for our ability to restore her alignment.
Discussion
The goals of spinal deformity surgery are restoration of regional and global alignment, achieving a solid arthrodesis while avoiding complications. Minimally invasive techniques can achieve reliable fusion rates while significantly reducing complications from blood loss, infections, postoperative discomfort and PJK. However, they are are often limited to shorter constructs and pathologies without significant sagittal deformity. One reason for the limited adoption for deformity surgery is that it is technically difficult to design and percutaneously deploy an instrumentation construct that predictably models and aligns the spine in 3 dimensions. We have found that with careful planning of the patient’s alignment and instrumentation construct with robotics, patient specific rods and decision support through AI, we have been able to reliably achieve our alignment goals without a large open procedure. It has been our experience that patients treated in this manner have experienced significant reductions in their complication rates compared to open procedures.