Robotic Guided Cervical Pedicle Screw Insertion Technique for Multilevel Cervical Spondylosis with Radiculopathy and Myelopathy.
Stanley Kisinde, MB.ChB, MMed;
Isador H. Lieberman, MD, MBA, FRCSC.
Patient History and Examination
A 75-year-old male presented with long standing history of neck pain and headaches. The neck pain was progressive and associated with a headache that he described as “wrapping around his head in a band-like formation”. Prior to this episode, he initially had neck pain that resolved following a C4-C5 and C6-C7 fusion operation. He is clear that the present type of neck pain is different from the initial one.
He also complained of progressively worsening left upper extremity weakness and occasional shooting pain into his left arm. He does have numbness in his left 5th and 4th fingers and EMG study done in July 2018 demonstrated severe left ulnar nerve entrapment as well as bilateral carpal tunnel syndrome.
He finds Sumatriptan and Tylenol helpful for the neck pain and headaches. He has also undergone several injections including Botox which were temporarily helpful.
He has a history of left rotator cuff repair in the 90s, multiple ulnar nerve surgeries and an L3 – L5 fusion in 2004.
Physical Exam
He presented wearing a cervical brace and had difficulty holding up his head without the brace, seen as the dropping of his chin to his chest, due to the fatiguing of the cervical muscles. He had well-healed anterior cervical surgical scars. He demonstrated a stooped forward posture and had difficulty in balance evidenced by a myelopathic / wide-based gait, difficulty with single leg stance and balance, and heel-to-toe walking. He however had a negative Romberg’s test.
The cervical muscles were non-tender with no evidence of spasm. Cervical spine range of motion was painful and restricted. He did have good range of motion of his right shoulder in flexion, extension, abduction and internal as well as external rotation, while he does have a Lt shoulder rotator cuff arthropathy with palpable and audible crepitus and limitation and restriction in range of motion.
Upper extremity strength was 4/5 in Lt biceps, triceps and deltoid muscles, and 3/5 for hand grip bilaterally; he had intrinsic muscle wasting in both hands. The sensation was intact to light touch and the reflexes were present and symmetric. The lower extremities revealed global deconditioning but no asymmetric motor weakness bilaterally.
Pre-operative Imaging:
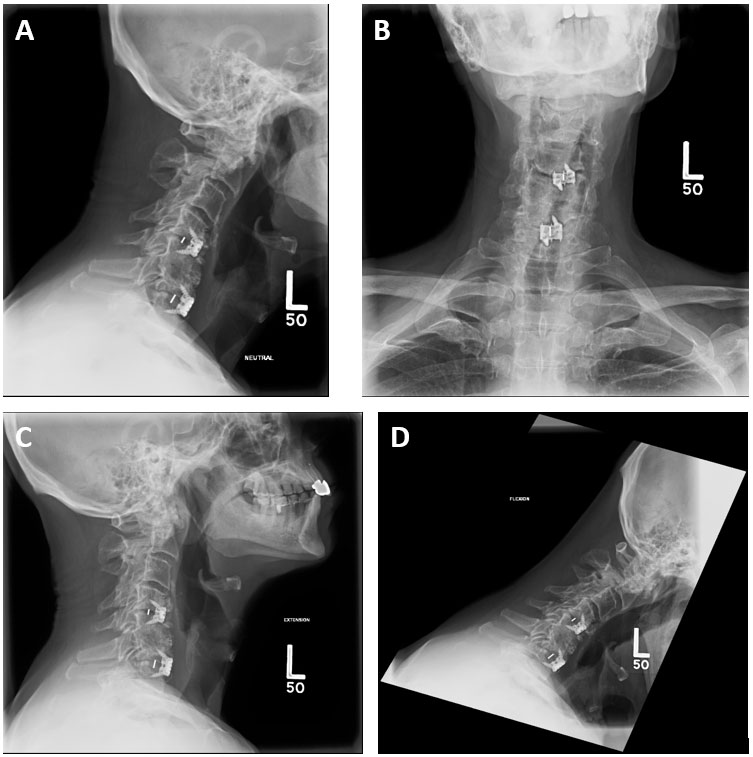
Figure 1: Cervical Spine Radiograph Images – Lateral (Neutral) (A), AP(B), Lateral (Extension and Flexion) (C & D respectively).
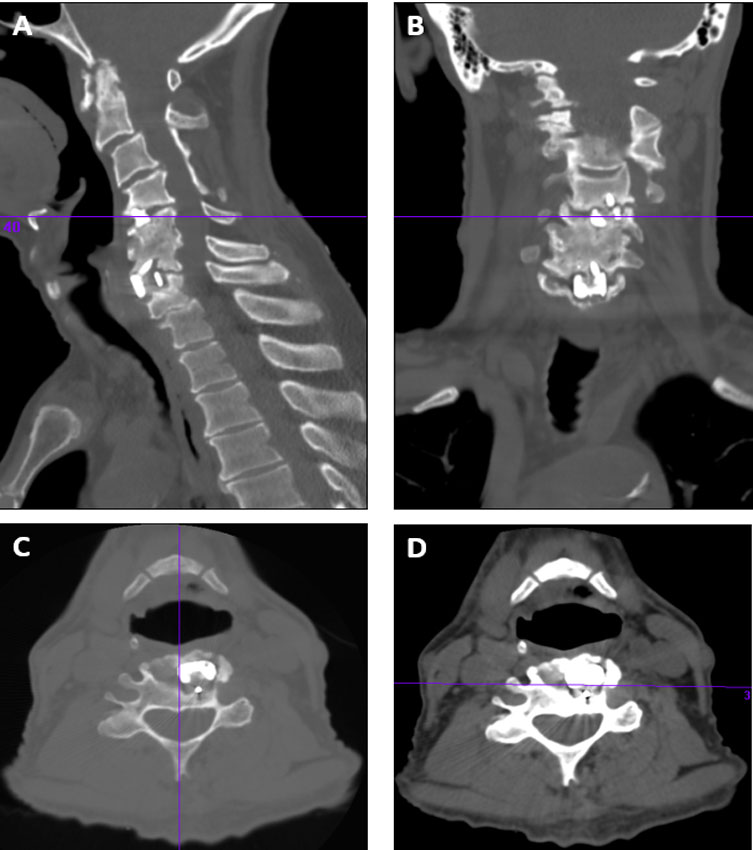
Figure 2: Cervical Spine CT Images reveal a previous anterior cervical discectomy and fusion at the C4-C5 and C6-C7 levels that have gone onto pseudarthroses. He also has an auto fusion at the C5-C6 level, end-stage degeneration at C1-C2, listhesis of C2 on C3 and C3 on C4, and listhesis and degeneration at C7 on T1 with central stenosis.
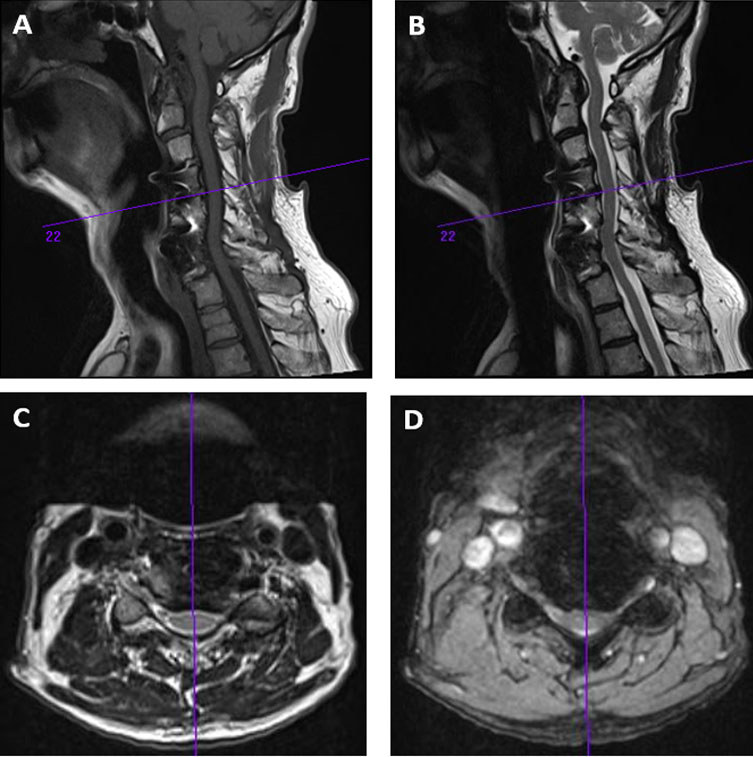
Figure 3: Cervical Spine MRI Scan Images – They also reveal listhesis and degeneration at C7 on T1 with central stenosis and cord impingement at that level.
Diagnosis:
The clinical picture is consistent with a drop head syndrome, along with neck pain and headaches, multiple level cervical spine central foraminal and lateral recess stenosis evidenced by left arm referred- and radicular pain as well as myelopathic signs and symptoms. His previous anterior cervical discectomy and fusion at the C4-C5 level as well as C6-C7 level have gone on to pseudarthroses. In addition, he has had previous left shoulder rotator cuff surgery and does have a rotator cuff arthropathy.
Treatment:
Goals:
-
Correct the deformity with instrumented fusion and relieve the stenosis with strategic decompression of the cervical spine.
-
The realignment of C2 on C3, and C3 on C4 will further provide for indirect decompression of the foramina and the stenosis.
Challenge:
- Revision surgery with distorted and / or complex anatomy, an autofusion of C5/C6 and pseudoarthrosis at C4/C5 and C6/C7.
Surgery selected:
A posterior C1-C2 to T2 pedicle screw instrumentation, correction and fusion with Smith-Peterson osteotomies and multilevel decompressions across C7 and T1 to facilitate realignment of the spine and alleviate the central foraminal and lateral recess stenosis, for his multilevel cervical spondylosis with radiculopathy and myelopathy, his multilevel pseudoarthrosis at C4-C5 and C6-C7, and his cervical kyphotic deformity.
Tips / Pearls:
-
A substantial correction was achieved and maintained with cervical pedicle screws.
-
If we had not achieved substantial correction, we would have had to resort to a staged anterior – posterior procedure.
Outcome:
Intra-op: – Successful
-
a. Pre-operative planning for the computer navigated robotic assisted placement of pedicle screws.
-
b. Bone marrow aspiration for bone graft slurry
-
c. Bilateral posterior spinal exposure from C2 to T2.
-
d. Computer navigated robotic assisted implantation of pedicle screw instrumentation from C2 through to C4 and C6 through to T2 on both the right and left sides.
-
e. Smith-Peterson / Ponte osteotomies at C7 – T1 and segmental correction of the deformity with rods attached to the screws from C2 through to T2.
-
f. Bilateral laminotomies at C7 and T1, and bilateral foraminotomies at C7 / T1.
-
g. Posterior and posterolateral spinal fusion from C2 through to T2.
Operative time / Surgical duration was 5 hours 40 minutes. EBL was 250 mls. No complications.
Peri-Op
He tolerated the procedure well and post op pain was controlled with medication. By the 7th day post operatively, he was stable and was discharged to a skilled nursing unit.
Long term
The patient recovered well with no symptoms or signs of wound infection. At 2 weeks follow-up, although the global upper extremity power was stable at 4/5, the hand grip strength improved from 3/5 to 4/5 bilaterally.
At 3 weeks follow-up, he reported substantial improvement in the left arm symptoms. There were still no wound issues.
By 3 months, he reported: good recovery, excellent results with physical therapy with regards to range of motion, global upper extremity strength at 4+/5, bilateral hand grip at 4/5 and hand intrinsic muscle strength at 3/5 on both sides. Sensation to light touch generally remained intact, reflexes alike, in the upper extremities. He ambulates with no assistive device.
His post-operative imaging (Cervical Spine CT scan images) reveal improvement in the cervical spine alignment (lordosis), increment in the size of the canal and proper positioning of the hardware.
The AP & lateral cervical spine radiograph images done at 3 months post-operatively revealed stable alignment, intact hardware and evidence of consolidation of the fusion.
Generally, he has recovered remarkably well thus far, his hands are functioning better, and he is mobilizing better as evidenced by the improvement in his VAS pain and NDI scores (See Figure 7 & 8).
Discussion:
The pedicle represents a robust point of attachment to the spine, and by traversing all three columns of the vertebrae, pedicle screws provide rigid stabilization of both the ventral and dorsal aspects of the spine. This allows for significant forces to be applied to the spine – pedicle screw complex without failure of the bone-metal junction. Furthermore, the rigidity of pedicle fixation allows for the incorporation of fewer normal motion segments to achieve acceptable stabilization of an abnormal level. Other important advantages of pedicle screw fixation include the facts that it does not require intact dorsal elements, includes less requirements for postoperative bracing and has thus far presented improvements in fusion rates.
(1) The cervical spine is unique due to limited surgical access in the face of naturally complex anatomy. There is also a smaller target bone volume for insertion of the transpedicular screws in this region, with important blood vessels and sensitive neural structures running intimately within the same bone complex.
(2) Therefore, there is a more crucial need for precision in pedicle screw insertion in this region, and robotic guidance technology provided us with the feasibility and accuracy relevant to this procedure.
Postoperative imaging
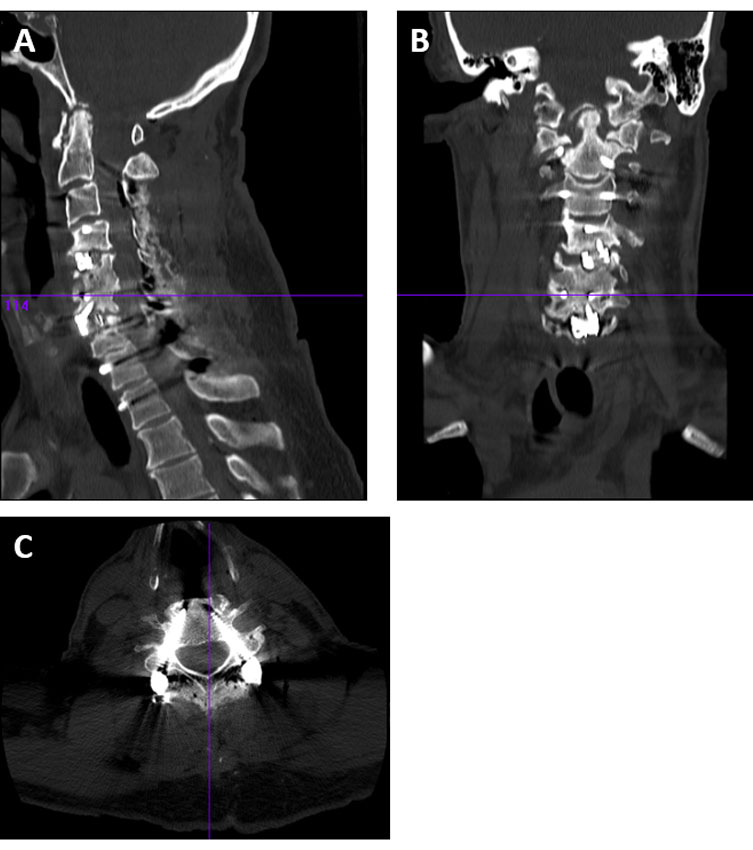
Figure 5: Immediate post op Cervical Spine CT Scan Images: A – Sagittal, B – Coronal, C – Axial cut at C6 showing accurately placed pedicle screws.
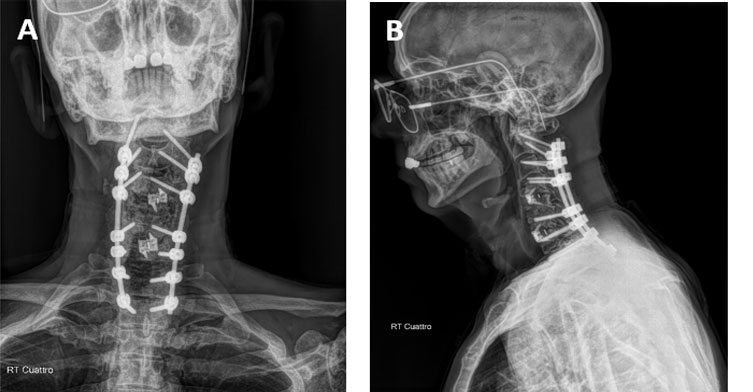
Figure 6: Post Op Cervical Spine Radiograph Images (A) AP and (B) Lateral. (3 months follow-up post-operatively). These images verify that the alignment has been maintained and the fusion is consolidating.
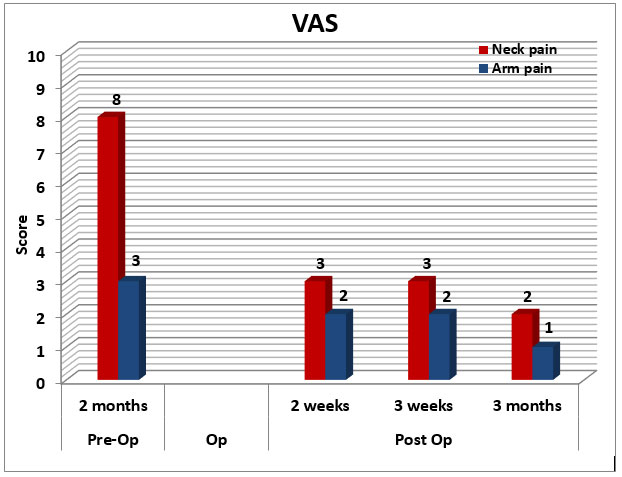
Figure 7: Graph showing Visual Analogue Pain Scores follow-up, pre- and post-operatively.
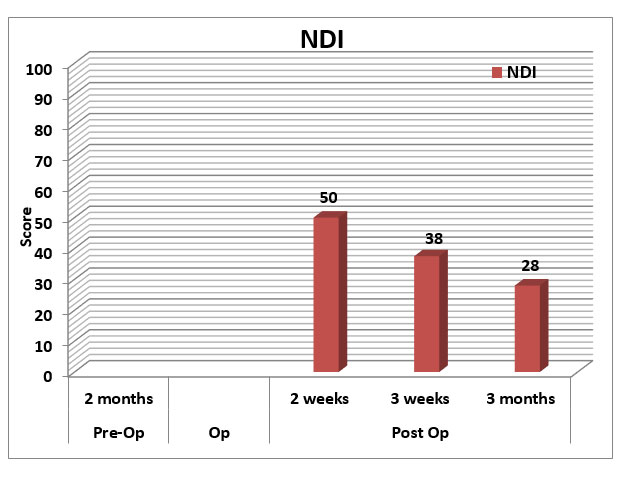
Figure 8: Graph showing Neck Disability Index Scores follow-up post-operatively.
References
-
1. Jeffrey Mullin MZ, Kevin M. Walsh, Edward C. Benzel. Benzel’s Spine Surgery: Techniques, Complication Avoidance and Management. In: Michael P.Steinmetz ECB, editor. Spine Surgery (Benzel). 4th ed. Philadelphia, PA: Elsevier; 2017. p. 717 – 28.
-
2. Roser F, Tatagiba M, Maier G. Spinal robotics: current applications and future perspectives. Neurosurgery. 2013;72 Suppl 1:12-8.