Single-Level Lateral Interbody Fusion for Sagittal Imbalance, Radiculopathy, and Iatrogenic Instability Due to Remote Flexion-Distraction Injury Status-Post Laminectomy
Alexander Butler, MD
Kern Singh, MD
Rush University Medical Center
Midwest Orthopaedics at Rush
This patient is a 59-year-old male who works as an accountant and enjoys recreational exercise. He presents due to slow progression of low back and bilateral thigh pain. With any prolonged standing, walking or other activity, this pain becomes severe and is associated with both lower extremity and postural fatigue. He relates a history of trauma at age 11, having been thrown from a horse and sustaining a lower back injury. At the time he was reportedly paraparetic, and was treated acutely with decompressive surgery. The patient has been able to manage occasional low back pain until the onset of his presenting complaints several years ago.
Figure 1: Standing XRays upon presentation demonstrate marked kyphotic deformity of the L4 body with accompanying distraction of the L3-4 posterior elements and segmental kyphosis of 33.6 degrees. Significant compensation at the adjacent lumbar levels negate much of the resultant relative global kyphosis, as a PI of 32.1 degrees and LL of 18.7 degrees yield a mismatch of 13.4 degrees.
.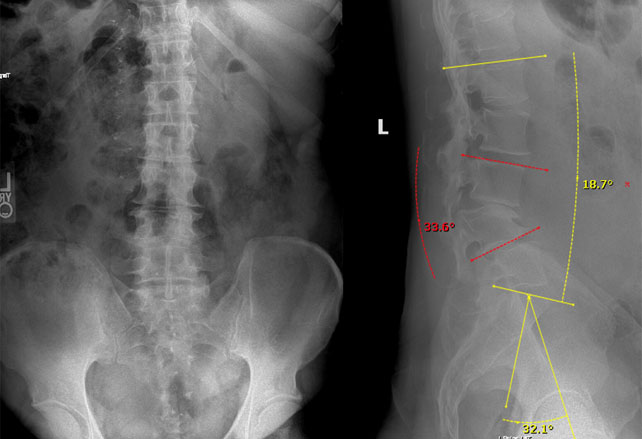
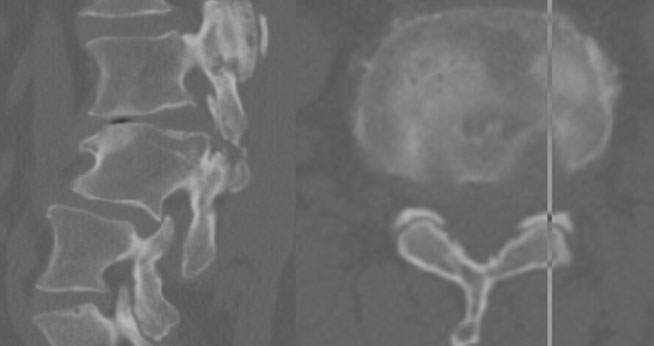
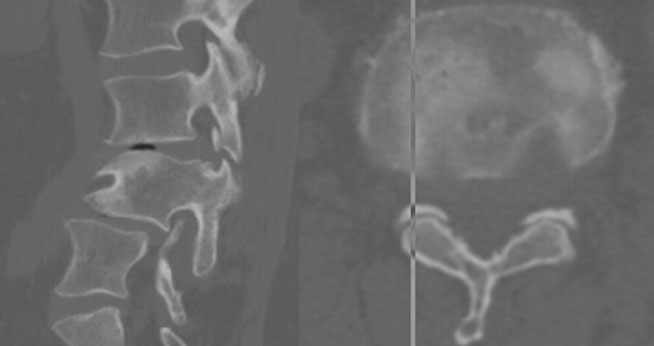
Figure 2: Pre-operative MRI reveals bilateral L3-4 foraminal, lateral recess and central stenosis with resultant nerve root clumping at the L3-4 level.
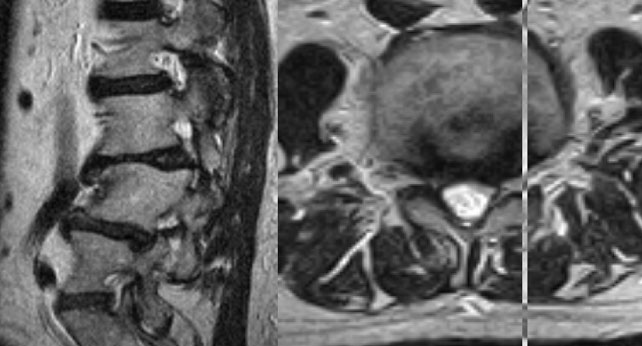
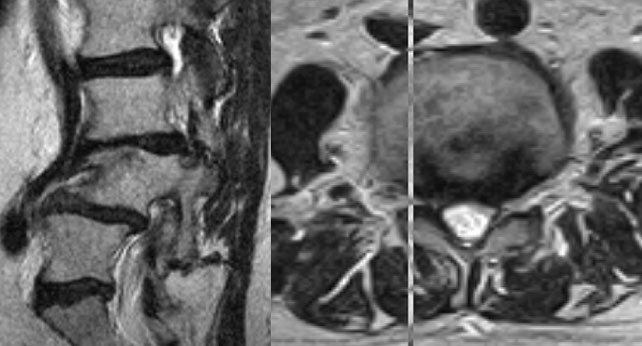
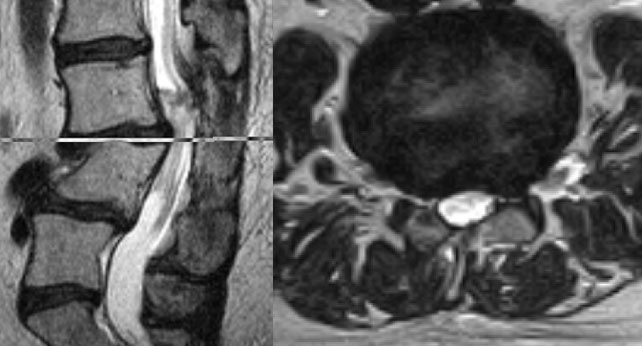
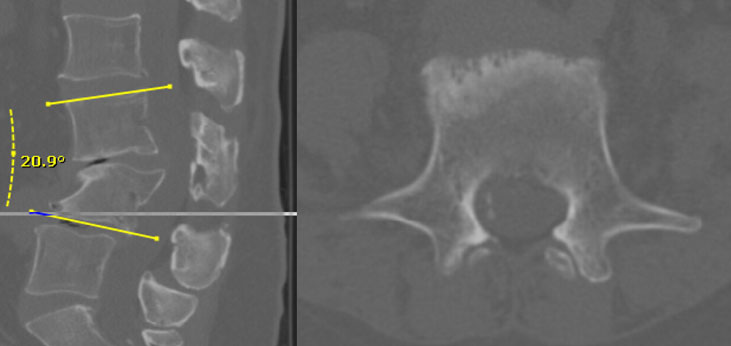
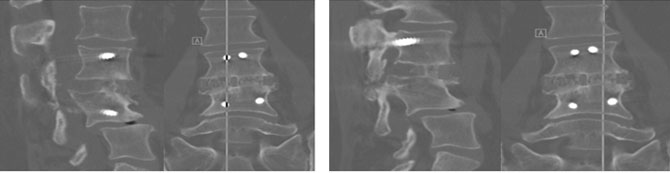
Figure 3: Pre-operative CT consistent with prior L4 laminectomy defect, and chronic distraction of the L3-4 facet joints. Partial correction of L3-4 segmental kyphosis as well as reduction in anterolisthesis in this supine image can be seen relative to the standing radiographs.
Diagnosis:
L3 radiculopathy and L3-4 spinal stenosis due to degenerative change superimposed on chronic, traumatic L3-4 kyphotic deformity and mobile spondylolisthesis with remote history of acute L4 laminectomy resulting in a component of iatrogenic instability.
Treatment:
L3-4 lateral interbody fusion with anterior column release and percutaneous posterior instrumentation
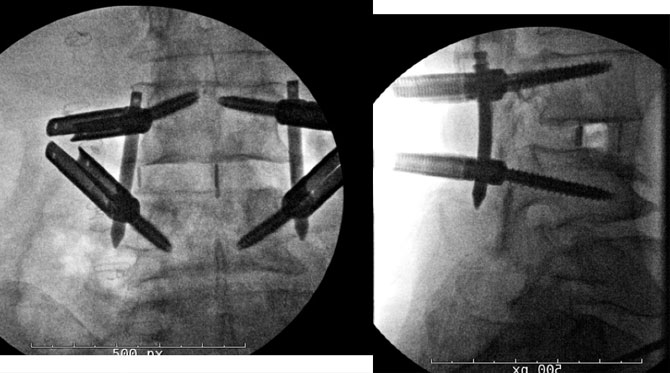
Figure 2: Intra-operative fluoroscopic images at at the conclusion of the procedure indicate anteriorly positioned lordotic, PEEK lateral interbody cage which has been stabilized by percutaneous pedicle screws and rods bilaterally.
Outcome:
The patients bilateral L3 radiculopathy had resolved entirely upon waking from surgery. He worked with physical therapy on POD0 and the morning of POD1 and described a marked improvement in walking tolerance and posture. Having been treated with a perioperative ERAS protocol, he experienced minimal pain and a decreasing narcotic requirement prior to discharge on on the morning of POD1. His functional status gradually improved to surpass his pre-operative baseline within 1-2 weeks after surgery, and by 3 months post-operatively he had returned to all desired activities without pain or limitation.
Figure 3: Standing lateral XR at 1-month (left) and 6-months (right) post-operatively demonstrate maintained segmental and global deformity correction.
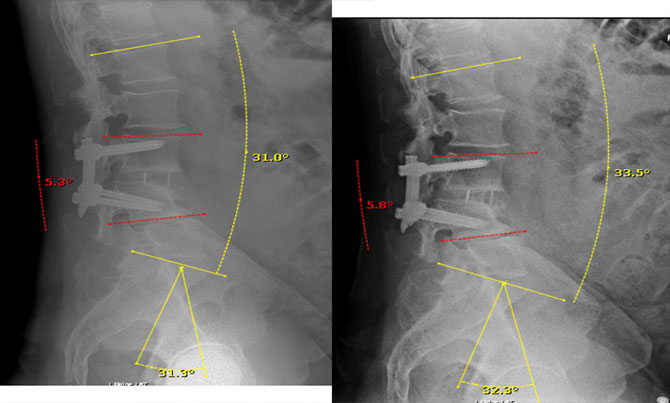
Figure 4: Sagittal and coronal CT images at 6-months postoperatively demonstrate uniform incorporation of end-plate to implant as well as bilateral columns of robust bridging bone through the cage consistent with successful inter-body fusion at the L3-4 level.
Discussion:
The goals of surgery were to decompress the L3-4 foramina and central canal, stabilize the mobile L3-4 anterolisthesis and improve global lumbar lordosis. These goals may have been accomplished predictably through a variety of techniques, though to do so while minimizing the local and systemic surgical footprint requires some planning and technical considerations.
Several factors led to the recommendation for a single-level lateral interbody fusion with anterior column release at L3-4. Avoiding a traditional posterior approach in this post-traumatic and previously decompressed spine was felt to be preferable to minimize surgical time and avoid a challenging revision decompression. A tall interbody implant was felt to be preferable to maximize indirect decompression through restoration of disc space height. The biomechanics of a large, lordotic interbody implant was also attractive to correct focal kyphosis and provide the best stability and fusion potential. Sharp release of the ALL from within the discectomy was desired to permit maximal focal correction via optimal implant placement and size. Intraoperative assessment of interference fit of the implant in the disc space was confirmed, and no lateral fixation was needed prior to repositioning prone for percutaneous pedicle screws.
There was pre-operative consideration of addressing the L4-5 level at the time of this index procedure given the retrolisthesis and likely contribution to loss of lumbar lordosis at this segment. However, unlike at L3-4, no L4-5 instability was noted on preoperative imaging. Additionally, neurologic symptoms corresponded with the radiographic description of isolated foraminal and central stenosis at L3-4. With regards to global alignment, preoperative planning allowed for an accurate prediction of segmental correction of 15 degrees by addressing L3-4 alone with an ACR as well as an appropriately placed and sized interbody implant. This would result in a matched LL and PI, indicating optimal sagittal alignment. Post-operative standing imaging indicates that this correction was indeed achieved, obviating the need for additional lordosis at adjacent levels.
The goals of surgery were met radiographically, and careful preoperative appraisal of symptoms allowed for a correspondingly excellent clinical outcome. Due to a targeted, minimally invasive approach, postoperative pain and inpatient stay were minimized, allowing for an accelerated course of rehabilitation and rapid return to desired activities.