Standalone Lateral for Adjacent Segment Degeneration
Isaac L. Moss, MDCM, MASc, FRCSC
Associate Professor of Orthopaedic Surgery and NeurosurgeryUConn Health Musculoskeletal Institute Comprehensive Spine Center.
History and Examination
This active, otherwise healthy 80-year-old woman presented with a 5-month history of progressive back pain, radiating to her right thigh and medial leg. She reports severe cramping in her legs when walking more than 20 yards, and sleep disturbances due to pain. As you can imagine, being in this much pain and without having to extensively move for it to occur, could be having a negative effect on her quality of life, as well as being limited in what she can do. To help control it, she may have already looked for different types of pain relief, such as the best CBD oils that she can find in her area, to help make sleeping and walking easier, or at least manageable. Luckily, her pain is able to ease at certain times as she reports complete pain relief when sitting. She had a successful TLIF at L4-5 for stenosis and spondylolisthesis in 1999.
Physical exam demonstrates a well healed lumbar midline incision. Posture is flexed forward when she ambulates. Motor and sensory exam of the lower extremities are normal.
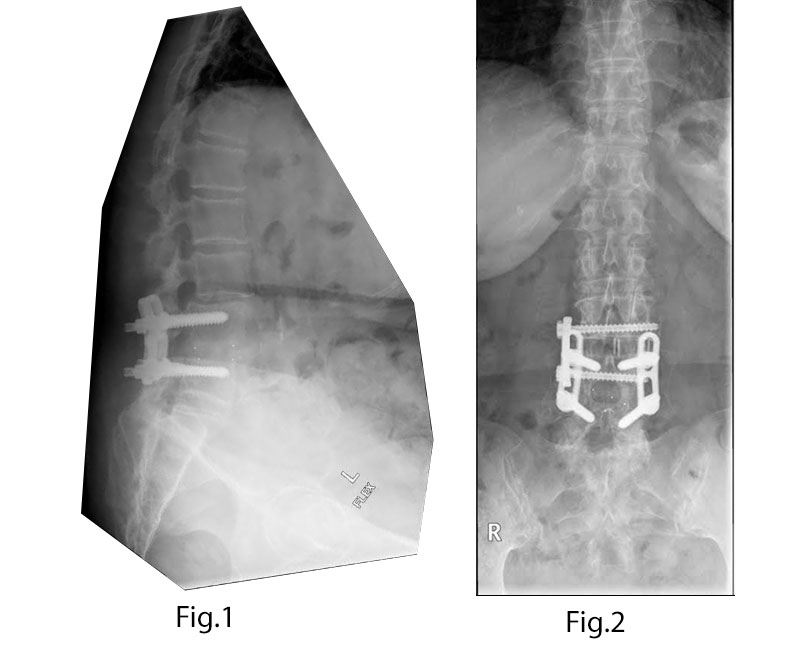
Pre-operative Imaging
Solid L4-5 fusion with interbody and Steffee plate construct. L3-4 Grade 1 spondylolisthesis with severe stenosis (Figs. 1-4).
Diagnosis
80-year-old woman with neurogenic claudication and radiculopathy due to L3-4 adjacent segment degeneration including spondylolisthesis and stenosis.
Treatment
Goal: Decompress and stabilize L3-4.
Challenge: Previous scar tissue and bulky hardware.
Surgery selected: L3-4 transpsoas lateral interbody fusion with insertion of an interbody device and supplemental lateral plate fixation. This approach was chosen to achieve indirect decompression to address the stenosis and stabilization to address the listhesis. This obviates the need for a direct decompression through a posterior approach, which would necessitate operating through significant scar tissue and/or the trauma associated with removal of hardware that has been in place for 15 years.
Pearl: Complete relief of radiculopathy at rest is generally a good indication that indirect decompression via the lateral interbody device will be adequate to address the patient’s stenosis.
Outcome
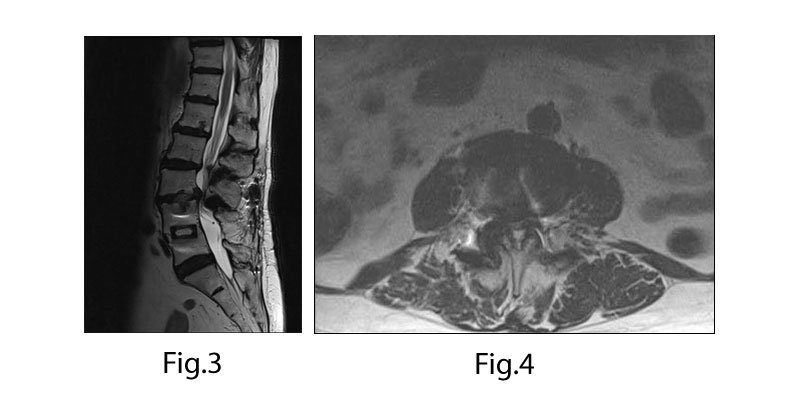
Intra-op: Successful transpsoas lateral fusion with 22mm wide, 10 mm tall interbody device and supplemental fixation with a lateral plate. Operative time was 40 minutes (23 minutes of psoas retractor time). EBL was ~25cc.
Peri-op: The patient mobilized on POD#0 with complete resolution of radicular symptoms, required only acetaminophen for pain control and was discharged to home on POD#1.
Long term: Symptoms remained resolved and the patient was able to walk 1 mile by 6 weeks post op. Follow up x-rays at 1-year post-op showed successful fusion (Fig.5).
Discussion
Revision surgery poses many challenges, including distorted anatomy, and scar tissue during the approach and within the epidural space. The need for hardware removal can also be a significant nuisance, due to tissue and bone overgrowth, and the difficulty in obtaining the appropriate tools necessary for disassembling a particular construct. The morbidity associated with an open posterior revision procedure can be avoided by addressing the pathology via an anterior or lateral interbody fusion to achieve indirect decompression and stabilize the motion segment. In this case, these goals were achieved with a standalone transpsoas lateral fusion, obviating the need to perform a posterior approach and causing minimal morbidity to an elderly patient.
