Thoracolumbar Non-Union Split Fracture Treated With MISS
Fernando Nin Vilaró, MD
History
28 y/o male. Healthy. 6-meter fall by explosion. Suffering several polytrauma, with chest and arms burns. Head trauma. Intense back pain and deformity and pain in both wrists.
Examination
Intense pain on thoracolumbar region, 3rd degree burns on chest and arms. Fracture syndrome of both wrists. Normal neurological exam. ASIA E.
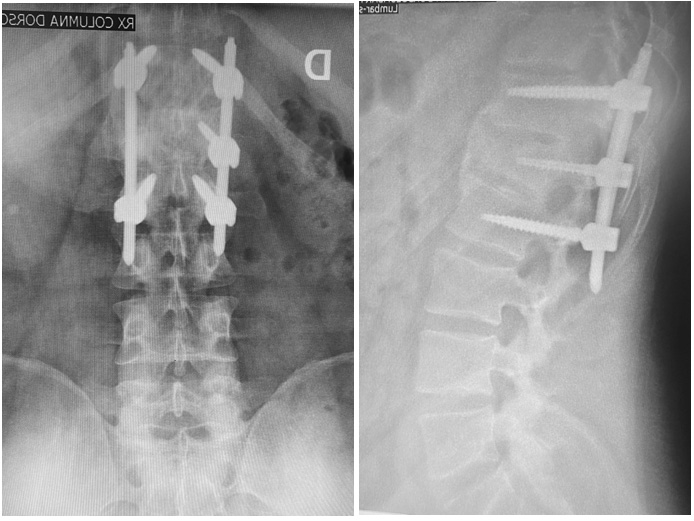
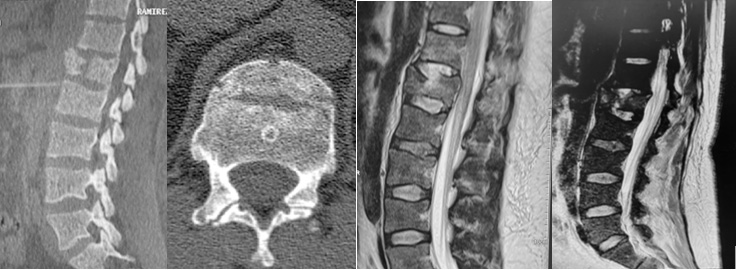
Imaging
CT Scan show L1 Split fracture in the sagittal and coronal plane. MRI show indemnity of posterior tension band and the rupture of the disc above.
Evolution
The patient went to ICU with diagnosis of thoracolumbar spine trauma, 3rd degree burns of the thorax and both arms. Chest trauma with pulmonary contusions and ribs fractures. ISS 36
Rest 88 days in ICU very unstable, severe respiratory failure with hemodynamic and kidney dysfunctions. Multiple respiratory, urinary, and skin infections.
He stabilizes at 3 months and authorized new evaluation.
The patient was very affected from the nutritional point of view. Albumin 3.4 g/dl Lumbar mechanical pain that becomes very intense when trying to ambulate. VAS 8/10. Normal Neurological examination.
New Imaging (3 moths after)
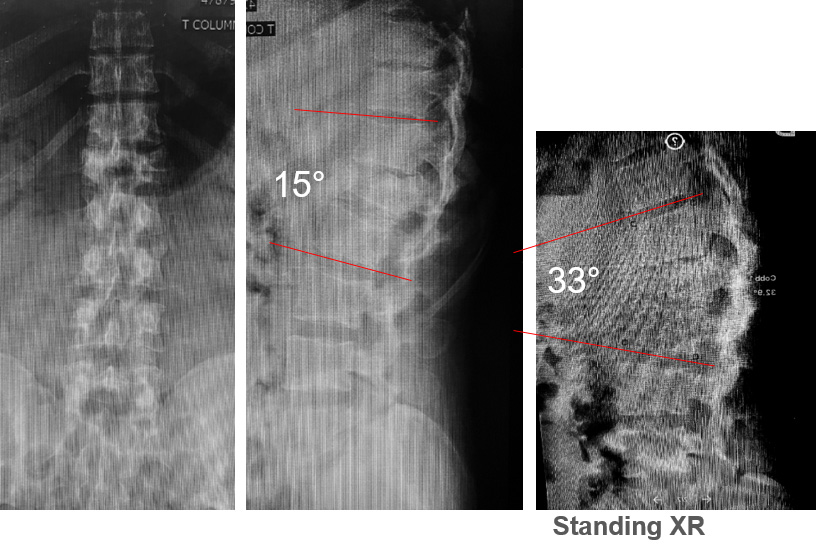

The new Imaging’s CT and MRI shows significant separation of the fragments with an earlier attempt at fusion between the vertebral bodies.
And we see the disk between the fragments in the MRI.
Discussion
We have 3-month evolution L1 A2 N0 fracture, with severe mechanical back pain with flexible deformity and a delay in the consolidation between the fragments with disk interposed. With high risk of infection.
Our primary idea was to make an anterior approach and them the posterior fixation.
The infectologist doctor suggests the least possible surgical approach due to the high risk of infection. Multiple respiratory, urinary, and skin infections with chronic colonization with KPC
Treatment
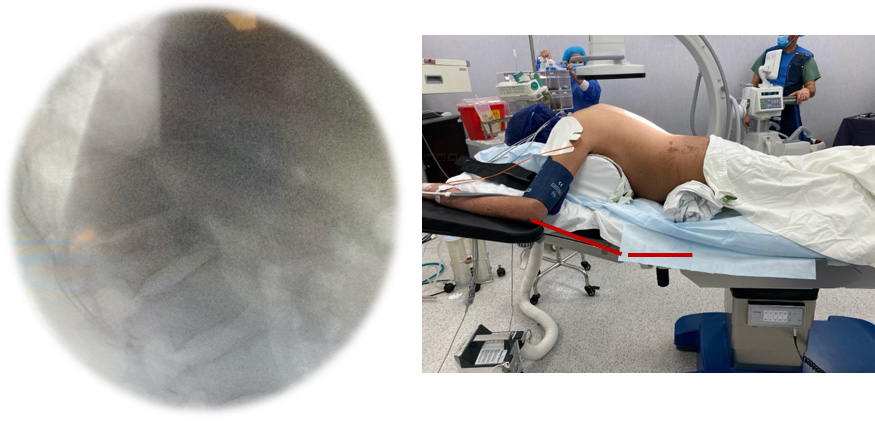
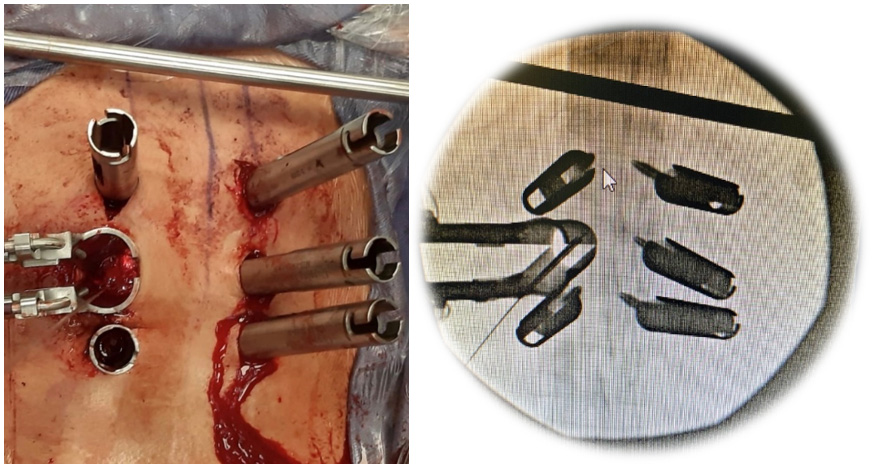
We propose a Posterior approach, MIS fixation and transpedicular curettage with iliac crest bone graft mix with substitutes.
We saw that we had good results with this technique, we avoided an anterior approach and its comorbidities. Always with the principles of minimally invasive surgery


Outcome
1 year
Without pain. Good function and fuse